Today technology has evolved to a point where patients either with normal refractive errors such as nearsightedness, farsightedness, astigmatism and presbyopia or those with ocular diseases that require specialized vision correction options such as those with keratoconus all have spectacular alternatives to maximize their visual performance. With the multitude of choices available, how does an individual make the decision which to take advantage of? Well let’s begin by saying that the input from your eye care professional is critically important. You need to be properly educated not only about the various options that are applicable to your individual situation but about the advantages and disadvantages of these options.
Normal Refractive Error Options
Let’s begin by discussing vision correction options available to those with normal refractive errors. Basically stated, these individuals have the ability to utilize spectacles, contact lenses or if they are appropriate candidates, consider the refractive surgical alternatives.
Glasses
Today spectacle lens technology has evolved to the point where exceptional vision quality can be achieved with lens designs that allow for the selection of almost any frame size or shape. Thin lens technologies have enabled those with high prescription powers to not only see amazingly well, but to wear glasses that remain quite thin and attractive even with some of the most extreme prescription powers. Your eye care professional can discuss the various lens material options that best work for your situation. New high index materials are not only thin but are very light weight. A concern for some however can be the significantly higher costs associated with these lens materials. For those who need multifocals, new digital and free form progressive addition lenses (PALs) have dramatically increased the success rates associated with adaptation to PALs.
Contact Lenses
Contact lens alternatives for those with normal refractive errors have also dramatically developed technologically over the past years. Today virtually every patient with normal refractive error is a candidate to wear contact lenses. Developments such as astigmatic contacts, multifocal contacts, and hybrid (rigid center / soft periphery) contact lens designs along with the introduction and the tremendous growth in the use of single use daily disposable contacts has made one form or another of contact lenses something to consider for almost everyone. Today’s CLs are healthier, more comfortable and provide better vision than ever before. CLs have the advantage of superior peripheral vision, more natural vision “sensation” and obvious advantages for demanding physical activities. With contemporary contact lens materials and designs we have successfully addressed issues that limited many people in the past such as concerns of poor comfort due to dryness, contact lens vision instability and contact lens induced complications associated with over-wear and over-use of lenses. Your eye doctor should always present contact lens options to you regardless if you ask or not. So often patients think that they can’t wear contacts, so it does become the responsibility of your doctor to inform and educate you about CL alternatives.

Combination of Glasses and Contact Lenses
So how do you decide if you should be a contact lens wearer or a glasses wearer? Who said you have to? The two vision correction options are not mutually exclusive; in fact they are quite synergistic. All contact lens wearers should have an excellent pair of glasses to use. Contacts may be more cosmetically acceptable to many, they may be much better for various physical activities such as sports, however there are many times when glasses may be preferred such as at the end of a long day of contact lens wear, first thing in the morning before inserting your CLs, or on those days you just don’t want to bother with your CLs or simply prefer the look of your glasses for some situations. Today even the person who predominantly wears glasses can consider part time contact lens wear. Single use daily disposable (DD) CLs are the perfect option for such an individual. DD CLs are now even available in astigmatism and multifocal designs!
Refractive Surgery
Refractive surgery is also developing and is more effective and safer today than ever before. An experienced and skilled eye doctor is in the best position to consult with you in order to determine if you are an excellent candidate for the various refractive surgical options available. Again, having refractive surgery does not always eliminate your need for glasses or contact lenses. Although that would be the optimal outcome, many patients still use glasses and contact lenses after having refractive surgery. Typically the glasses and contact lenses are far less strong and are used significantly less often than prior to surgery. Some patients need them due to complications of surgery while others need them when outcomes did not perfectly correct vision and of course refractive surgery does not stop eyes from changing over the years, so many patients who had successful refractive surgery may experience vision changes years after surgery that require the use of glasses, contacts or both.
Irregular Refractive Error Options
Specialty Contact Lenses
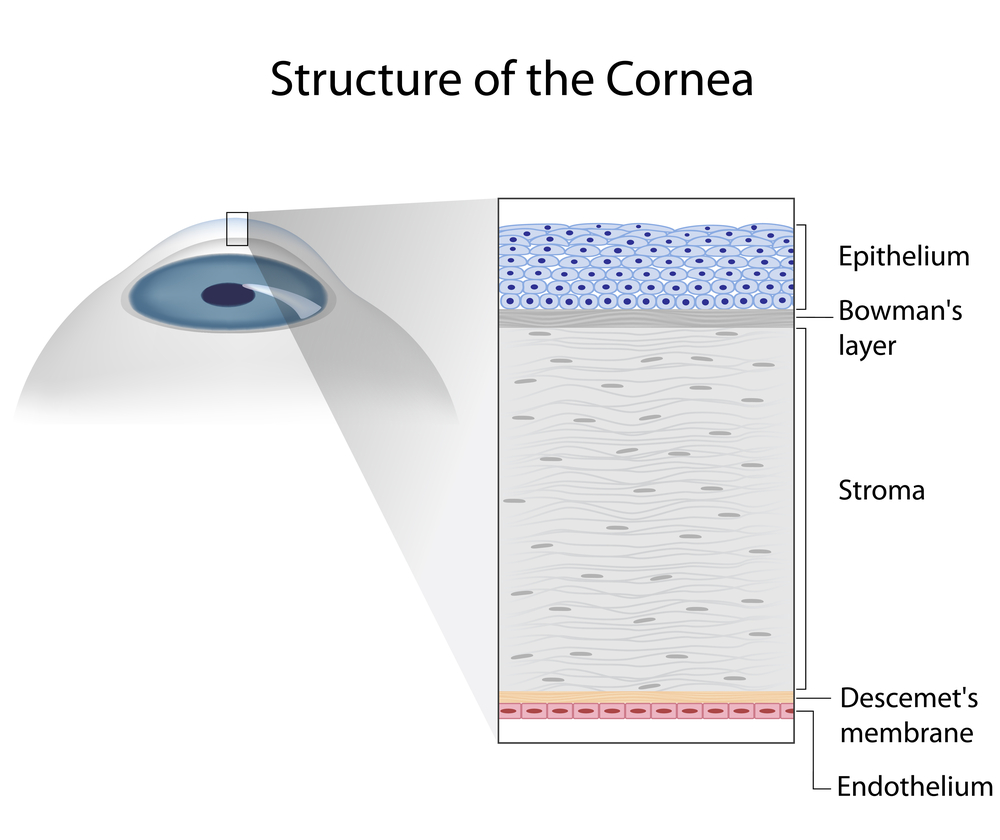
Next let’s talk about choices in vision correction for those with irregular corneas and other conditions that are termed “medically necessary” vision correction cases. Individuals with irregular corneas such as those with keratoconus or post LASIK or other refractive surgery induced ectasias often require contact lenses that in essence “mask” the irregularity of the cornea. In the past this equated with the fitting of rigid corneal contact lenses, however today many other alternatives can be considered such as the fitting of scleral large diameter gas permeable contacts, hybrid CLs designed for irregular corneas and even combination systems of soft lenses with corneal gas permeable lenses (called “tandem” or “piggyback” CL systems). These CL alternatives provide advantages such as improved comfort, improved eye health response by limiting contact lens to cornea bearing, and improved contact lens positioning and stability which positively impacts visual performance.
Combination of Contact Lenses With Glasses
It should be clearly stated that spectacle lens alternatives still can have a significant role in the treatment of individuals with irregular corneas. Often glasses can be prescribed that provide adequate vision if even for part time and limited applications. While less severe cases may perform quite well with glasses as their primary modality of vision correction. Your doctor may need to modify the power of your glasses prescription in order for you to adapt to wearing glasses, however even a modified prescription power can frequently allow for some degree of visual function and allow for the ability to reduce the number of contact lens wearing hours during the day.
Surgical Procedures
Application of certain surgical and medical procedures such as intra-corneal ring segments (Intacs TM) or corneal collagen cross linking (CXL) for corneal irregularity can often help these patients in various ways and may allow for perhaps a less complex contact lens application or easier adaptation and improved function with glasses. Management of these diseases and conditions is quite complex and requires the expertise of doctors with extensive experience. Your doctor, if appropriately skilled and experienced can provide you with all of the required information and education so that you both can jointly decide on the best vision correction options for you.
In conclusion, patients today have numerous options for their vision correction. These options each have advantages and disadvantages but in most cases can be utilized synergistically. The role that your eye care professional plays in consultation and education of the vision correction alternatives applicable to you cannot be over stated. Vision is a precious gift and you should experience the highest quality of visual performance possible.
2/26/15
 S. Barry Eiden, OD, FAAO
S. Barry Eiden, OD, FAAO
Medical Director, North Suburban Vision Consultants, Ltd.
NSCV Blog: www.nsvc.com/blog
President and Founder, International Keratoconus Academy of Eye Care Professionals