The Brain and the Eye
The eye works like a camera. The iris and the pupil control how much light to let into the back of the eye, much like the shutter of a camera. When it is very dark, our pupils get bigger, letting in more light; when it is very bright our irises constrict, letting in very little light.
The lens of the eye, like the lens of a camera, helps us to focus. But just as a camera uses mirrors and other mechanical devices to focus, we rely on eyeglasses and contact lenses to help us to see more clearly.
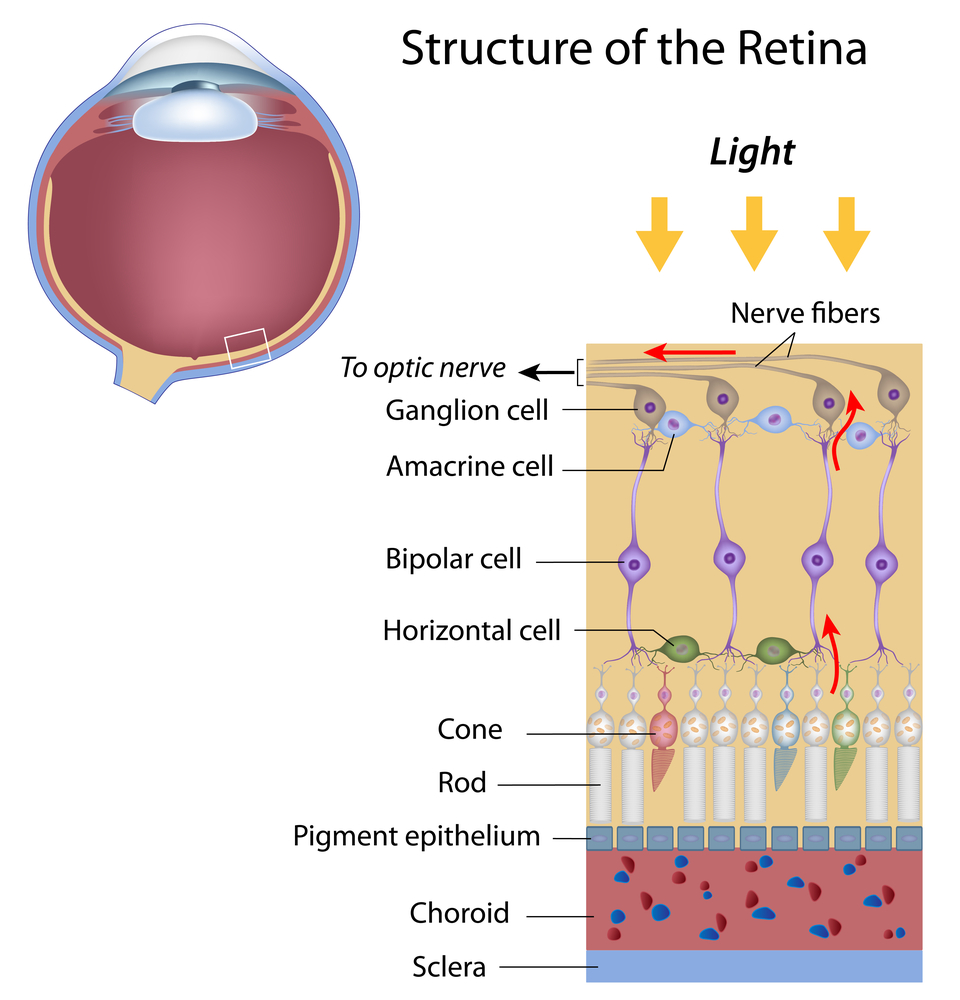
The focus light rays are then directed to the back of the eye, on to the retina, which acts like the film in a camera. The cells in the retina absorb and convert the light to electrochemical impulses which are transferred along the optic nerve to the brain. The brain is instrumental in helping us see as it translates the image into something we can understand.
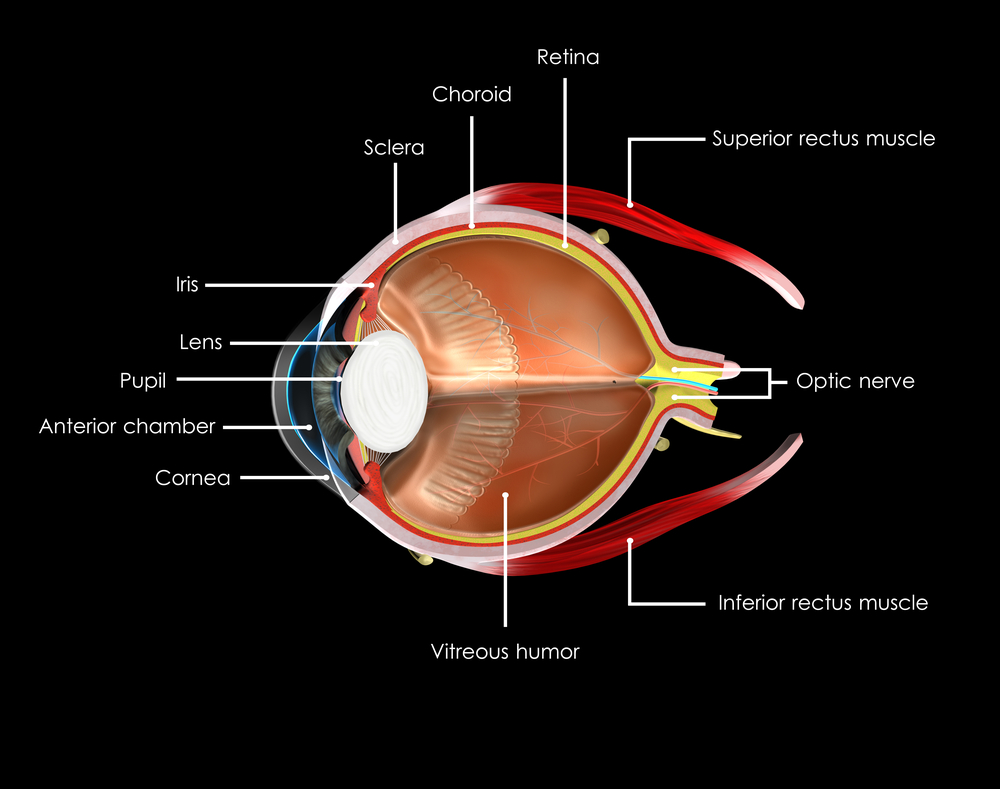
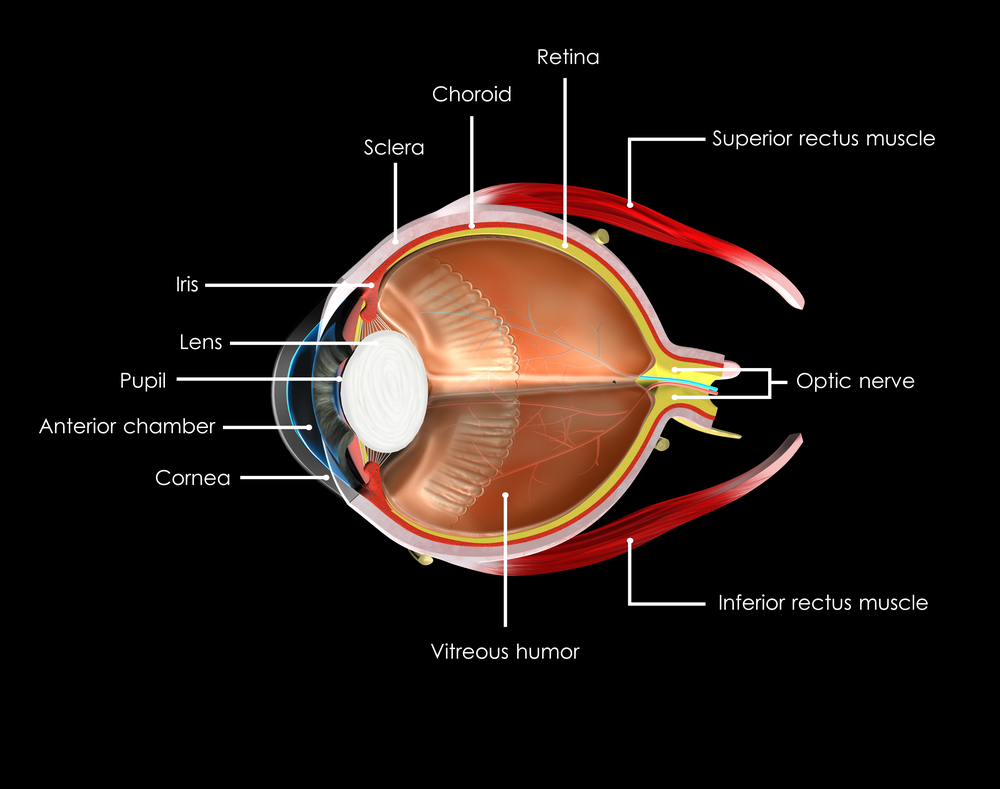
The eye may be small, but it is one of the most amazing parts of your body. To better understand it, it helps to understand the different parts and what they do.
Choroid
A layer with blood vessels that lines the back of the eye and is between the retina (the inner light-sensitive layer that acts like film) and the sclera (the outer white part of the eyeball).
Ciliary Body
The muscle structure behind the iris, which focuses the lens.
Cornea
The very front of the eye that is clear to help focus light into the eye. Corrective laser surgery reshapes the cornea, changing the focus to increase sharpness and/or clarity.
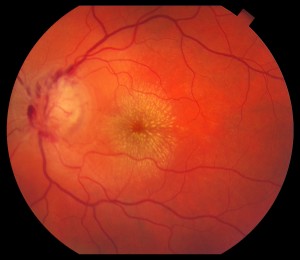
Fovea
The center of the macula which provides the sharp vision.
Iris
The colored part of the eye used to regulate the amount of light entering the eye. Lens focuses light rays onto the retina at the back of the eye. The lens is transparent, and can deteriorate as we age, resulting in the need for reading glasses. Intraocular lenses are used to replace lenses clouded by cataracts.
Macula
The area in the center of retina that contains special light-sensitive cells, allowing us to see fine details clearly in the center of our visual field. The deterioration of the macula can be common as we age, resulting in age related macular degeneration.
Optic Nerve
A bundle of more than a million nerve fibers carrying visual messages from the retina to the brain. Your brain actually controls what you see, since it combines images. Also the images focused on the retina are upside down, so the brain turns images right side up. This reversal of the images Is a lot like what a mirror does in a camera. Glaucoma can result when increase pressure in the eye restricts the flow of impulses to the brain, causing optic nerve damage and makes it difficult to see.
Pupil
The dark center opening in the middle of the iris changes size to adjust for the amount of light available to focus on the retina.
Retina
The nerve layer lining the back of the eye that senses light and creates electrical impulses that are sent through the optic nerve to the brain.
Sclera
The white outer coating of the eyeball.
Vitreous Humor
The clear, gelatinous substance filling the central cavity of the eye.
3/3/16
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation