Thanksgiving is almost here; a meal that nourishes the family bonds and traditions. It’s the one time of the year where you can guarantee your eyes will be bigger than your stomach. This meal also has another added bonus — almost every item on the Thanksgiving table is healthy for your eyesight!
Here are several of the most popular Thanksgiving dishes and their corresponding benefits to your eye health:
Turkey –
No Thanksgiving is complete without a turkey, roasted golden brown and stuffed with fresh vegetables and herbs. Turkey is loaded with zinc and B-vitamin niacin, which helps prevent the formation of cataracts. Cataracts are the leading cause of vision loss in the United States, so gobble up! You are “preventing” cataracts with every bite.
Spinach, Green Bean Casserole, Asparagus and Brussel Sprouts –
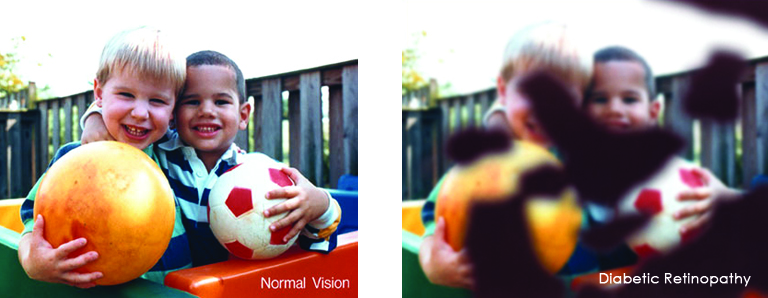
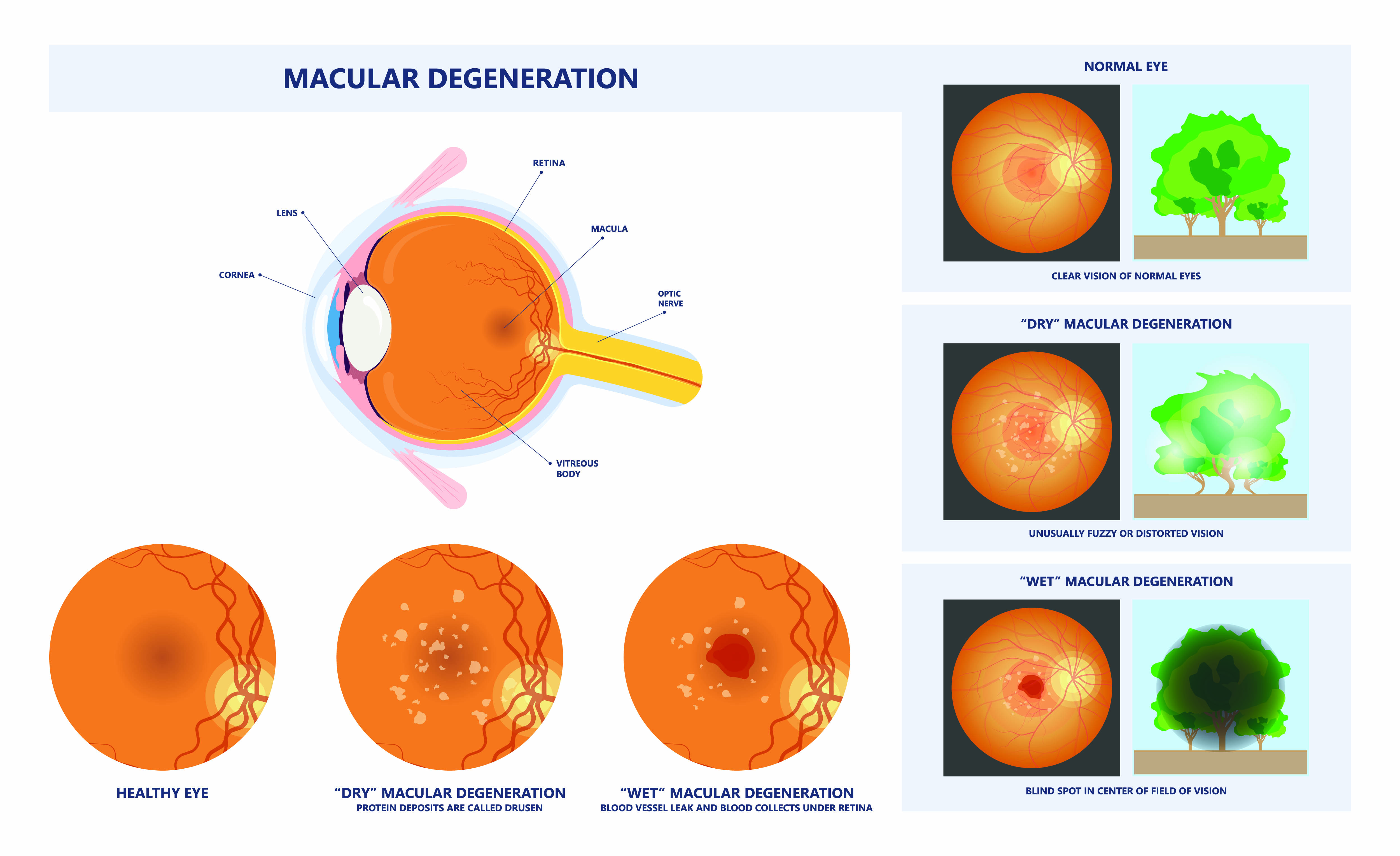
These foods and other leafy greens are loaded with lutein and zeaxanthin, two nutrients that protect the retina, which may also help reduce the risk of cataracts and macular degeneration. Healthy Green Bean Casserole Recipe
Sweet Potatoes –
Sweet potatoes are full of Beta-carotene, which is a carotenoid and antioxidant that promotes night vision and overall good eyesight. Sweet potatoes are also loaded with vitamins C and E. Diets that are rich in these vitamins can help prevent or delay the development of cataracts and macular degeneration. Mashed Sweet Potatoes Recipe
Cranberry Sauce –
Cranberries contain bioflavonoids, a large class of antioxidants. Bioflavonoids are found in the pulp, skin and rinds of foods that contain vitamin C. Both flavonoids and vitamin C help protect the eyes from free radical damage caused by pollution and the body’s normal metabolic processes.
Pumpkin Pie –
Pumpkin is one of the best sources of vitamin A, so pumpkin pie is an eye-healthy dessert. In fact, one cup of cooked, mashed pumpkin contains more than 200 percent of the recommended daily intake of Vitamin A. Vitamin A provides nourishment and protection to the eye’s lens, cornea and macula (part of the retina), so it improves night vision.
A diet that’s full of the right nutrients is a great start to keeping your eyes healthy, but don’t forget that regular eye exams are equally important! We hope you enjoy a happy and delicious Thanksgiving with family and friends.
*For more eye healthy recipes click here EYE COOK


 Make sure they take frequent screen breaks. Instead of focusing directly on the screen, encourage your child to look around the room every now and then, or take some time to stare out the window (at least 20 seconds is recommended by the American Optometric Association). You can even remind them to blink.
Make sure they take frequent screen breaks. Instead of focusing directly on the screen, encourage your child to look around the room every now and then, or take some time to stare out the window (at least 20 seconds is recommended by the American Optometric Association). You can even remind them to blink. It’s easy for us to forget about our eyes let alone our child’s, but it is very important to get your child’s eyes checked regularly.
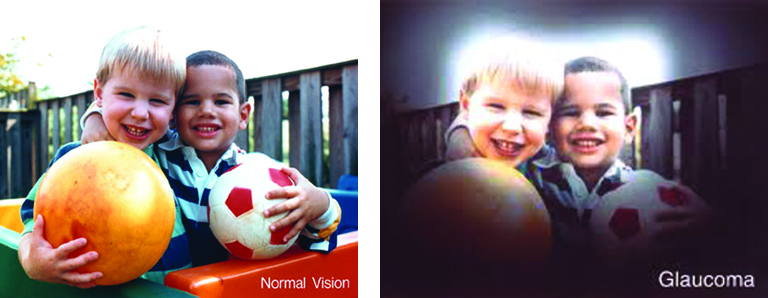
It’s easy for us to forget about our eyes let alone our child’s, but it is very important to get your child’s eyes checked regularly. Most people have eye problems at one time or another. Some are minor and will go away on their own, or are easy to treat at home. Others need a specialist’s care. Some eye issues come with age while others may be a serious condition.
Most people have eye problems at one time or another. Some are minor and will go away on their own, or are easy to treat at home. Others need a specialist’s care. Some eye issues come with age while others may be a serious condition. Dry eye is a common condition that occurs when your tears aren’t able to provide adequate lubrication for your eyes. Tears can be inadequate for many reasons. For example, dry eyes may occur if you don’t produce enough tears or if you produce poor-quality tears. Dry eyes can also feel very uncomfortable.
Dry eye is a common condition that occurs when your tears aren’t able to provide adequate lubrication for your eyes. Tears can be inadequate for many reasons. For example, dry eyes may occur if you don’t produce enough tears or if you produce poor-quality tears. Dry eyes can also feel very uncomfortable.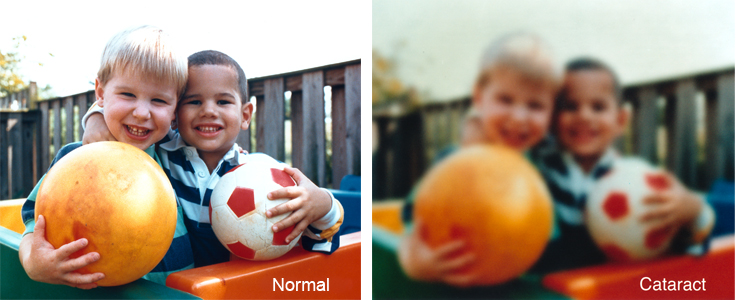

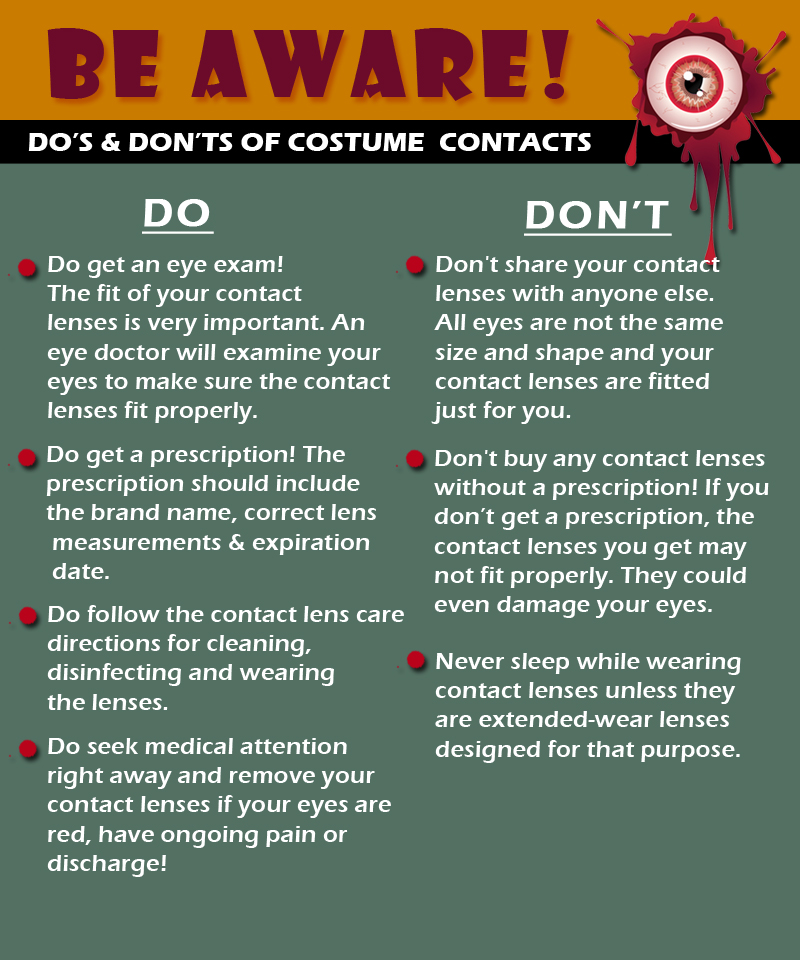
 Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.
Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.