Summer time is officially here and everyone enjoys a dip in a nice, cool pool during the summer months. While swimming is a great form of exercise and a relaxing way to cool down, the water can be hard on your eyes.
Summer time is officially here and everyone enjoys a dip in a nice, cool pool during the summer months. While swimming is a great form of exercise and a relaxing way to cool down, the water can be hard on your eyes.
What Chlorine Does to Your Eyes –
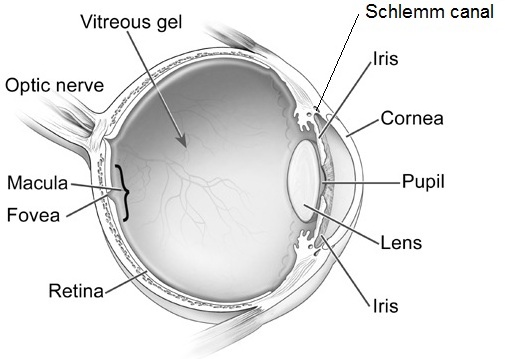
Yes chlorine can make your eyes red! But the real dangers in pool water aren’t just a result of your eyes coming in contact with the chemical. The redness and discomfort that sometimes accompany swimming can be caused by bacteria that linger in the water. When submerged in chlorine-treated water, your eyes lose the tear film that protects against infection. Even though the purpose of chlorine in pools is to reduce the amount of harmful bugs, some contaminants are resistant to the chlorine that is used. This means the health of your eyes can be compromised with infections caused by bugs still lingering in the water.
This can result in these three common eye issues:
- Pink eye or conjunctivitis – This is one of the most common eye infections swimmers can get, as it can be either viral or bacterial and spreads quickly and easily through the water.
- Red, irritated eyes – This is a result of your eyes becoming dehydrated due to the chlorine and the removal of your tear film. Sometimes you may also experience blurriness and distorted vision, this is usually only temporary.
- Acanthamoebic keratitis – This is a severe eye infection that is caused by amoeba in the water becoming trapped between the cornea and the contact lens. It can begin to live there, which can result in ulcers on your cornea and permanent damage to your vision.
Swimming with Contact Lenses
Wearing contact lenses in any type of water—including a pool, hot tub, ocean or lake—puts you at higher risk for a corneal infection. Bacteria and other microbes can grow on the lenses even after just one swim. Because contact lenses sit on your eyes for an extended period of time, your eyes are then continuously exposed to chemicals, bacteria, fungi or parasites after you swim. That can lead to a painful infection, corneal damage, and even loss of vision.
To avoid any kind of infection, remove contacts altogether when swimming or use swim goggles. You can get prescription swimming goggles to help keep your vision clear and eyes healthy in the pool. Talk with your eye care provider for more information about the different kinds of swim goggles available.
If you have any of these eye infection symptoms are increasing one hour or longer after swimming, see your eye doctor right away.
Redness
Pain
Tearing
Being very sensitive to light
Blurry vision
Sensation of having something in your eye
Discharge from your eye
Eye swelling
With all of these risks to your eyes from chlorine, swimming might seem a bit scarier than before. However, there is no need to panic! By taking a few safety measures, you can protect your eyes and still enjoy your time in the pool.
 Wear Goggles – Wear a pair of swim goggles every time you swim. Goggles keep pool chemicals out of your eyes.
Wear Goggles – Wear a pair of swim goggles every time you swim. Goggles keep pool chemicals out of your eyes.
 Wash Your Eyes – Immediately after swimming, splash your closed eyes with fresh tap water. This washes chlorine and other chemicals off your eyelids and eyelashes.
Wash Your Eyes – Immediately after swimming, splash your closed eyes with fresh tap water. This washes chlorine and other chemicals off your eyelids and eyelashes.
 Use Eye Drops – Use over-the-counter lubricating eye drops before and after swimming to keep the tear film balanced and eyes comfortable.
Use Eye Drops – Use over-the-counter lubricating eye drops before and after swimming to keep the tear film balanced and eyes comfortable.
- or Use Gel Tears – If you have dry eye, thicker artificial tears called gel tears will help protect your tear film, use these drops before putting on your goggles.
 Stay Hydrated – Don’t forget to drink plenty of water. Staying well hydrated is an important part of keeping your eyes moist and comfortable.
Stay Hydrated – Don’t forget to drink plenty of water. Staying well hydrated is an important part of keeping your eyes moist and comfortable.
Don’t miss out on the fun this summer! By taking these easy steps whenever you decide to take a dive, you can have peace of mind that your eyes and your vision are protected.



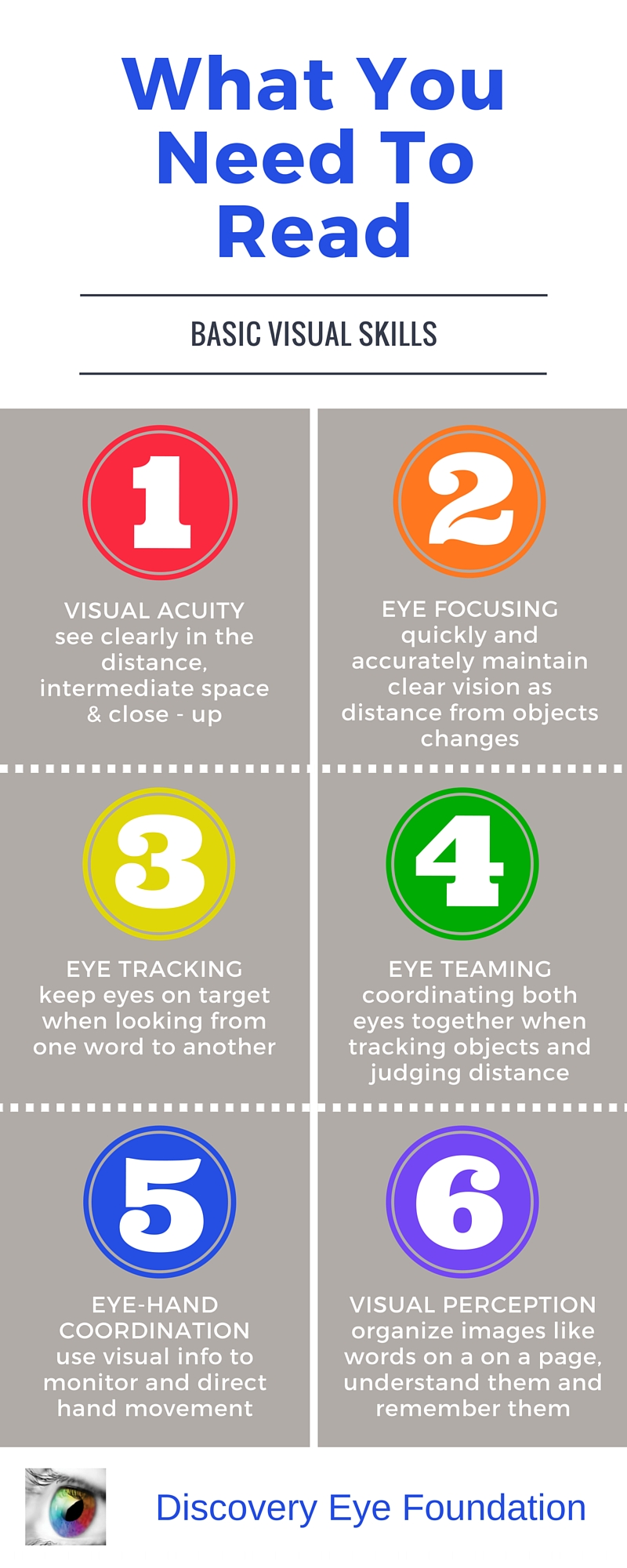
 Summer is almost over and it’s back to school season. As parents, many of us are busy ensuring our kids are ready and prepared for the new year; worrying about school supplies, new clothes, and new haircuts. There is always a long list of things to do before school starts. But something that often gets overlooked is getting your child’s eyes examined annually.
Summer is almost over and it’s back to school season. As parents, many of us are busy ensuring our kids are ready and prepared for the new year; worrying about school supplies, new clothes, and new haircuts. There is always a long list of things to do before school starts. But something that often gets overlooked is getting your child’s eyes examined annually. Vision loss is feared more than the loss of any other sense and is considered to affect the quality of life more than most other issues. When it comes to children, even partial vision loss can be damaging because it can affect the way that your child learns and develops. There are several different types of issues that may affect your child’s vision. Awareness is key to prevention and treatment.
Vision loss is feared more than the loss of any other sense and is considered to affect the quality of life more than most other issues. When it comes to children, even partial vision loss can be damaging because it can affect the way that your child learns and develops. There are several different types of issues that may affect your child’s vision. Awareness is key to prevention and treatment. Amanda Duffy
Amanda Duffy